Women are constantly experiencing shifts in the body-- physically and mentally. More than just obsessing over gray hair and wrinkles, however, the symptoms become more traumatic and problematic as ladies get older.
"I haven't met many women over 30 who aren't suffering from brain fog, fatigue, irritability, mood swings," said founder of Evexias Health Solutions Terri DeNeui, NP.
For a lot of women, the first symptom is that they can't sleep through the night. For others, the frustration centers around image.
"I think the biggest thing that affects women is... they can't lose weight after 35 or 40 when they used to be able to when they were younger," said Dawn Cutillo, 51. Cutillo is author of "The Hormone Shift."
Women tend to believe that these dips in energy, sexual vitality or overall interest are just something that happens to everyone because of age.
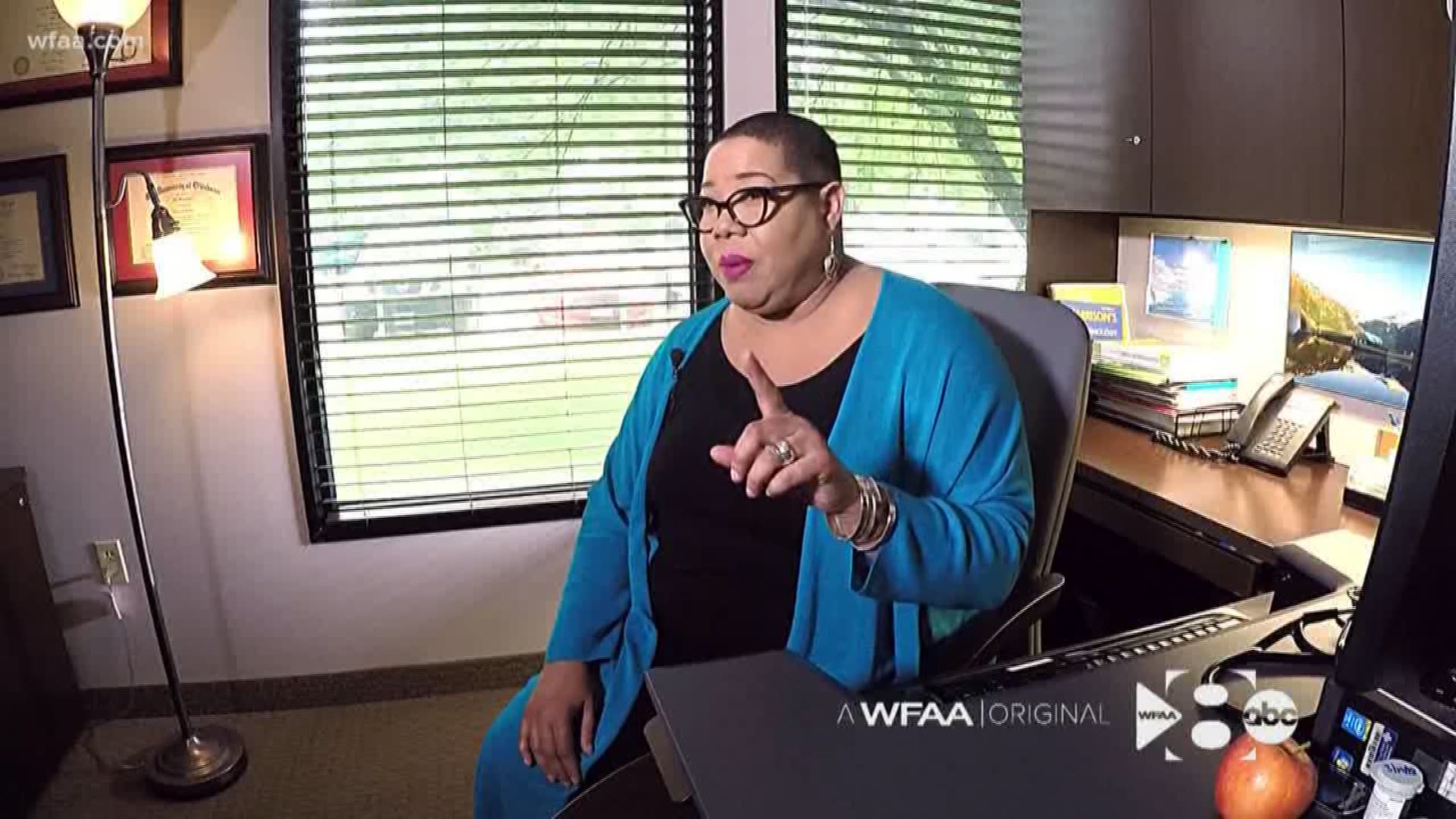
"It's not everyone," said Dr. Jill Waggoner. "And it doesn't have to be everyone." Waggoner is a 60-year-old practicing board-certified family medicine physician in Dallas.
Hormone imbalance can happen many years before the dreaded hot flashes and night sweats, said DeNeui, especially for those who have had children in their 20s.
"There's a genetic component to it; there's a lifestyle component to it," said Waggoner. "We know there are things that cause you to age quicker."
Those factors include: alcohol, smoking, poor diet and lack of exercise. Additionally, now more than ever we are outpacing our bodies.
"If you're under more stress, it's going to drain hormones and cause more problems with mood, weight and sleep," said Cutillo, who is founder of BeBalanced Centers. She offered a quick lesson: we all have estrogen, testosterone and progesterone -- hormones that are always fluctuating. But as we age, women experience particularly dramatic natural drops in progesterone, which keeps us in check and in estrogen which is responsible for our brain function, sex drive, even skin texture.
Cutillo said that hormone replacement therapy has evolved beyond what to many is still perceived as dangerous.
"Synthetic hormone replacement therapy has kind of been deemed by the FDA as a little bit unsafe," Cutillo said. "Use the smallest amount for the shortest amount of time possible."
Fast forward to what's popular now: bio-identical hormone replacement therapy.
"The term, which some people argue with, simply means the chemical structure of the hormone that you're getting... looks like what you take in your body," Waggoner explained. "The thought is your body is able to process it better. The receptors will recognize it if it looks the same as what you make in your body."
Hormone pellets are particularly prevalent. Both Waggoner and DeNeui get them, on average, like most women four times per year.
"It's the closest thing that we've found to mimic the body's natural production of hormones," DeNeui explained from her Southlake medical center.
Pellets as a hormone therapy option have been around since the 1930s. They are similar to compounded hormone powders that you would find in some cream, pills or patches, but instead placed under the skin.
"It's pressed down into this tiny pellet that's about the size of a rice grain, and it's released based on cardiac output. It's not time released," DeNeui said. "So the more active you are... the more you exercise... the more stressed you are- good stress or bad stress- that'll determine how fast you blow through them."
DeNeui and Waggoner were careful to caution women who receive hormones without proper research.
"We don't just look at [you and say] ok, your gas tank is empty, so we're going to put some hormones in your system and hope for the best," DeNeui said. "You really want to find somebody who can get to the root cause. There's a lot of band-aids out there."
Waggoner echoed her sentiment.
"If you are going to do hormones, you need to know what your levels are," Waggoner said. "Otherwise you may be putting yourself in danger."
A baseline blood or saliva test should help you to figure out a good starting point. Too much estrogen could stimulate breast or endometrial tissues. Too much testosterone could lead to feature changes and facial hair, Waggoner elaborated.
Cutillo added that it is possible to balance hormones without drugs or surgery. BeBalanced is one of the newest weight loss centers in Dallas.
"Just lifestyle changes, education, support and some natural supplements," Cutillo said. "Lower the stress, balance the hormones and they can literally look and feel better when they're 50 than when they were 45."
Waggoner said that while women can't avoid the dreaded years before and during menopause, it is possible to transition gracefully.
"You know, there are people who say anti-aging," said Waggoner. "I don't think I can stop aging. But I think we can age differently. We can age with vigor, and focus and write and run... and play with our grandchildren, and just enjoy life."
Information on menopause hormone therapy and compounded drugs is available on the FDA's website. Compounded drugs are not FDA approved.
The FDA released the following statement to WFAA:
The FDA is particularly concerned about compounded hormone drugs promoted as “bio-identical hormone replacement therapy (BHRT).” Some pharmacy compounders claim that their compounded “BHRT” drugs are a “natural” alternative to FDA-approved drugs, because the compounded hormones are purportedly identical to the hormones produced in the body. The FDA is not aware of any credible scientific evidence establishing these claims, nor is the FDA aware of sound evidence showing that the side effects and risks of compounded “BHRT” drugs that use estrogen and progesterone as active ingredients are different than those of similarly formulated FDA-approved menopausal hormone therapy drugs.
Compounding can be an important component of patient care. However, compounded drugs, including compounded drugs that contain hormones, are not FDA-approved. This means that they have not undergone premarket FDA review of safety, effectiveness, or manufacturing quality. Compounded drugs can pose health risks. For example, compounded drugs made using poor quality compounding practices may be sub- or super potent, contaminated, or otherwise adulterated. Therefore, when an FDA-approved drug is commercially available, the FDA recommends that practitioners prescribe the FDA-approved drug rather than a compounded drug unless the prescribing practitioner has determined that a compounded product is necessary for the particular patient and would provide a significant difference for the patient as compared to the FDA-approved commercially available drug product.
Furthermore, with regard to bioidentical hormones, the adverse events most commonly associated with these products, like those related to conventionally manufactured hormones, which include breast cancer, strokes, blot clots, and heart problems, are likely to occur only after years of use, and the patient may not connect the event with the hormones they have been taking. Because these adverse events are relatively common in the population of women who use these products, epidemiological studies would be needed to detect an increase in the adverse events associated with these products that were distinguishable from the relatively high background rates of these events.
The FDA encourages health care professionals and consumers to report adverse reactions associated with these or similar products to the agency’s MedWatch program.