This story originally appeared in The Texas Tribune.
As Texas sets records for new COVID-19 cases and hospitalizations day after day, the state’s hospital capacity — one of the key metrics that Gov. Greg Abbott cited as he allowed businesses to reopen — has become the focus of increased attention and concern.
But the state isn’t releasing the information it collects about how many beds individual hospitals have available. And only a fraction of the state’s hospitals, cities, and counties are providing that information to the public on their own.
The Texas Department of State Health Services has that data at its disposal. Hospitals across the state have been sending daily reports on how many available regular and intensive care unit beds they have, as well as the number of available ventilators, to regional health authorities, which send the information to the state. The agency then publicly releases that data for the state as a whole and for the state’s 22 trauma service regions.
Data for individual hospitals or counties is not made public “because hospitals within trauma service areas coordinate to ensure their communities have necessary care, and because people often cross county lines to get hospital care,” said Chris Van Deusen, a DSHS spokesperson.
Hospital officials in Houston and other parts of the state recently warned that hospitals could get overwhelmed if the number of infections keeps climbing. Statewide, 6,904 patients in Texas were hospitalized with COVID-19 on Wednesday — a figure that has been going up nearly every day since June 1.
On June 25, Abbott reinstated a ban on elective surgeries in four counties that are seeing rapid increases in coronavirus cases, saying he remains focused on maintaining sufficient hospital capacity; three days earlier, he told Texans that hospital capacity was “abundant.” The governor expanded the ban to four more counties in South Texas on Tuesday.
According to data from DSHS, the state had 1,322 available intensive care unit beds and close to 13,000 available hospital beds Wednesday. But there are important regional disparities. The Northeast Texas Regional Advisory Council reported Wednesday that 43% of its hospital beds are in use with 92 ICU beds available, while the East Texas Gulf Coast Regional Advisory Council, which includes nine counties and more than 1.3 million people, is 83% full with only 10 open ICU beds.
Some of the regional advisory councils provide county-level breakdowns of available hospital beds within their boundaries, including the Southeast Texas Regional Advisory Council, which includes Houston.
Many local government and health authorities have opted not to make hospital capacity information public.
“Publicly, we do not share which hospitals are at capacity, because there is constant shifting and we want the hospitals to have the freedom to move resources as needed,” Mark Escott, Austin's interim public health authority, said in an email.
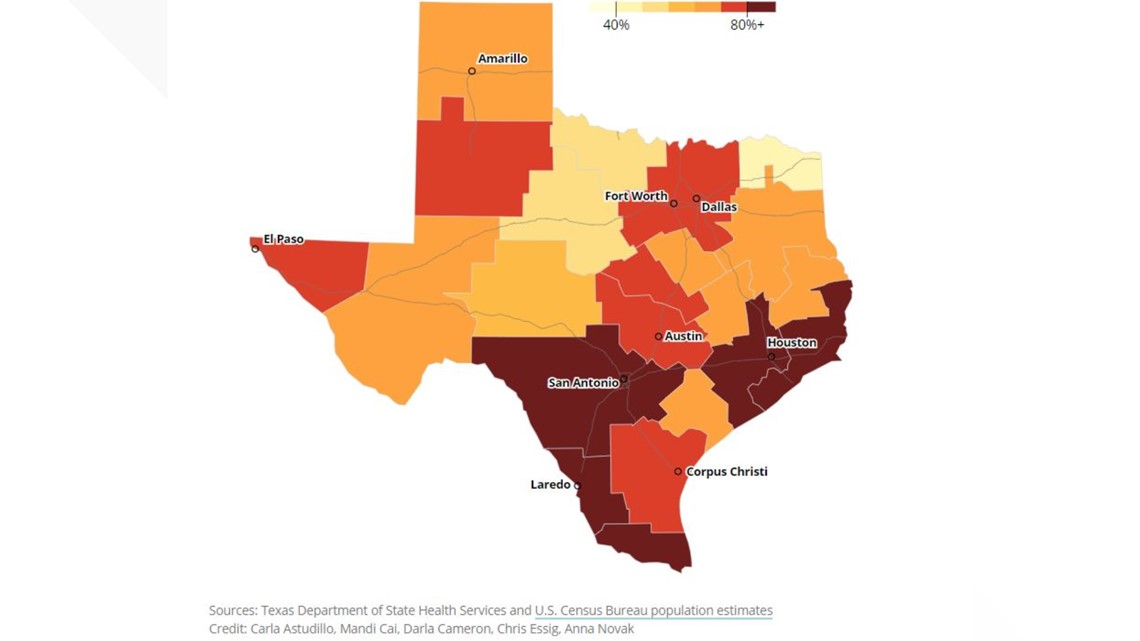
Hospital beds in use in Texas
The Texas Tribune is tracking the percentage of hospital beds in use for each trauma service region, which shows the strain the coronavirus can put on hospitals across different parts of the state. These regions are administered by Regional Advisory Councils (RACs).
RELATED: See other maps and charts

Dallas County provides daily briefs that include hospitalizations, ICU admissions and emergency room visits — but doesn’t include available hospital capacity — saying local health experts use these key indicators to determine the COVID-19 risk level and the appropriate response.
The Texas Medical Center in Houston, which includes 21 hospitals, used to update daily a set of “early warnings,” including its base intensive care capacity. On June 24, TMC leaders issued a statement warning that patients with COVID-19 were being admitted at an “alarming rate.” The next day, the medical center reported it had reached 100% of ICU base capacity — and then stopped updating that information for almost three days.
During a joint news conference June 25, Houston Methodist CEO Dr. Marc Boom said officials were concerned that the level of alarm was “unwarranted.”
The Houston Chronicle reported that Abbott had expressed displeasure to hospital executives about headlines related to ICU capacity, but Abbott spokesman John Wittman said any insinuation that the governor suggested the executives publish less data is false.
“We were getting panicked calls from elected officials and members of the media saying, ‘You all are out of ICU beds, what are we going to do?’” David Callender, president and CEO of the Memorial Hermann Hospital, told KHOU-TV. “We were not doing a very good job with our slides and portraying how we manage our capacity.”
The slides that the medical center posts on its website have been changed to put emphasis on its available surge capacity.
But the sudden change in data reporting brought criticism from Harris County Judge Lina Hidalgo.
“The timing is suspect. I find it very very problematic,” Hidalgo said in a new conference Monday. She said that her team uses this data to help develop its projections and that the county’s message urging residents to stay home can be “diluted” by this sudden change.
Although the hospital capacity data is available to state and county officials, some local agencies say they are in the dark about capacity at their own hospitals.
The Austin Public Health Department, which organizes COVID-19 response locally, does not “yet have a data feed from all of the hospitals in the [area] to accurately determine daily occupancy and capacity,” a spokesperson said.
Last week, Sarah Eckhardt, the former Travis County judge serving as an adviser to interim County Judge Sam Biscoe, said she was having trouble obtaining information about capacity at local private hospitals. On Tuesday, she said that the county has since received all the information it needs to plan its response to the recent surge in COVID-19 hospitalizations, which reached 369 in Travis County on Tuesday, including 132 people in ICU.
Travis County has a 22.9% positivity rate, a figure “substantially higher than most of the country,” Escott said in a news conference Wednesday. The positivity rate is the ratio of positive cases to the number of tests conducted, and it can vary depending on who is being tested, health experts say. Public testing in the county is being rationed to only people with symptoms.
“I think that it's pretty plain that if the chief executives of the county and the city are having a hard time getting information about the occupancy levels in the hospitals, then how would you expect the regular individual to know?” Eckhardt said.
The Texas Tribune is a nonpartisan, nonprofit media organization that informs Texans — and engages with them – about public policy, politics, government, and statewide issues.
More on WFAA:
- What will the long-term effects of COVID-19 pandemic be on our nurses?
- Personal video diaries give glimpse into COVID-19 fight at Parkland Hospital
- Cook Children's reports more than half its positive COVID-19 cases have come over the past week-and-a-half
- Dallas County's Clay Jenkins hopes for new mask mandate, stay-at-home order as cases and hospitalizations continue to break records



