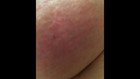
ROCKWALL – Breast cancer doesn’t always present itself as a tumor or lump. For Jennifer Cordts, it was a tinge of redness similar to a sunburn on the side of one of her breasts.
"I really want this to educate. I really want someone to say, 'Oh my gosh, I have redness in my breast. I better push past the mammogram and ask for some more tests,'” said Cordts, 46, a mother of two daughters.
Jennifer’s journey began two years ago after recognizing the slight discoloration. She alerted her primary care doctor, who ordered a test.
"I went and got a mammogram and it came back normal. Everything looked fine," she explained.
The mammogram showed no lump, no tumor, and her blood work was normal. Her doctors dismissed it. So did she. It was a relief.
"I was told, crazy enough, that my bra was too small," she recalled as a reason given by her doctor.
But after buying new bras and taking an antibiotic prescribed by another physician, the light red spot on her breast did not go away.

One night as her husband and youngest daughter slept, Jennifer typed her symptom into Google.
"IBC came up. Inflammatory Breast Cancer,” she said. “It was the first thing that popped up. And it was late at night. Everybody was asleep. And I was terrified. I just had a bad feeling."
After 11 months of misdiagnosis, a biopsy confirmed what a mammogram could not.
"It took my breath away," she said, recalling when the radiologist told her the diagnosis. "I remember him saying 'inflammatory breast cancer.' And all I could think about was what I Googled. Because what I Googled said everybody dies. That nobody survives. So I knew my fate right then."
It was stage four IBC.
Despite the diagnosis, Dr. Joyce O’Shaughnessy at Texas Oncology inside Baylor University Medical Center is treating Jennifer. Medicine cannot stop her inflammatory breast cancer but has successfully slowed it down.
Researchers have not determined what causes IBC. It makes up one percent of all breast cancers and unfortunately, it's often diagnosed too late.
"The doctors gave us three to five years. That was a year and a half ago. We're hoping for five, right?," said Rob Cordts, Jennifer’s husband.
Every three months though, anxiety sets in for the couple. It’s when Jennifer must get a scan to see if the cancer is spreading.
"You're trying to stay positive for the kids and the wife but I cry every day," said Rob, 46.
Adding to the anxiety of the scan, it takes another week to learn the results.
"Everything's going to be fine,” Rob told his wife in a private moment in the waiting room. “You gotta stay positive OK? You gotta fight. Right?”
He kissed her forehead as she wiped away tears.
“It's OK," he whispered.
"Here's the thing. This is so rare that many gynecologists and primary care providers – they don't see this stuff. They don't see it so they'll come up with every excuse that it's something else than what it is. This is how it goes undetected,” said Dr. Shannon Poppito, a clinical psychologist at Baylor Scott & White.
Like many similar patients, Jennifer's treatment is as much mental as it is medical.
She sees Dr. Poppito at Baylor Scott & White in East Dallas every other week.
"The head and the heart is 90 percent of the battle because she's carrying around with her the awareness that she will die from this cancer,” added Poppito.
Jennifer’s life is now about making memories.
She and her family are planning an Alaskan cruise.
Jennifer met her sister in Las Vegas for a Celine Dion concert recently, and took her 7-year-old daughter Daisy to see the beach for the first time.
"I wouldn't be truthful to you or anybody else if I didn't say I was sad. And maybe a little mad. But mostly sad," said Cordts.
Still, she wants this story to warn other women to push for more tests if they’re concerned.
“I'm not necessarily afraid to die, but I'm very afraid to say goodbye," she said.
It’s one fear she never expected to face.

